“Chronic Lyme disease” is a term that still generates controversy in the medical world.
I was recently interviewed by Charles Seales of Newsy’s “The Why,” who asked me what I’d say to people who claim chronic Lyme disease is not a legitimate diagnosis. I also spoke with him about the findings of our recently published study on Lyme disease.
Newsy is an online national news network.
View the video interview on chronic Lyme disease.
Charles Seales: What's to be done for chronic sufferers who, many times, confound their doctors? Are we getting any closer to a solid diagnosis, and more importantly, an effective treatment, whatever the diagnosis? I asked Lorraine Johnson, she's the CEO of lymedisease.org, which advocates for research and treatment of Lyme.
Charles Seales: We hear the medical community, not all of it, but major parts of it, say chronic Lyme disease is not a legitimate diagnosis. Do you think that will ever be resolved?
Lorraine Johnson: I think it will be resolved. I think there's been an enormous amount of movement towards recognition of how serious chronic Lyme disease is. I think the CDC stepping in and recognizing it has been really important, but I think those people recognize that there are a lot of patients who aren't diagnosed early. In MyLymeData, we have 70% of the patients are not diagnosed until late, and these are patients who have late or chronic Lyme disease, so they have symptoms, like 45% had early symptoms. There was a real opportunity to get in, make a diagnosis quickly, treat those patients promptly and restore them to health. Most patients who are treated early get well.
Charles Seales: Many times, we hear that mood disorders or neurological problems are co-morbid, and it's thinking that that's what's driving this, but in fact, what you're saying is maybe undiagnosed Lyme disease has actually spurred that.
Lorraine Johnson: No, that's exactly right. So what happens is, people are misdiagnosed with depression, or they're misdiagnosed with chronic fatigue, or they're misdiagnosed with fibromyalgia, they're misdiagnosed with MS, they're misdiagnosed with a disease that has no cure, and that's a real missed opportunity because maybe they're being given, then, palliative care, things that relieves symptoms instead of something that addresses the underlying cause.
Charles Seales: What is the best treatment in your opinion, or what are you asking for?
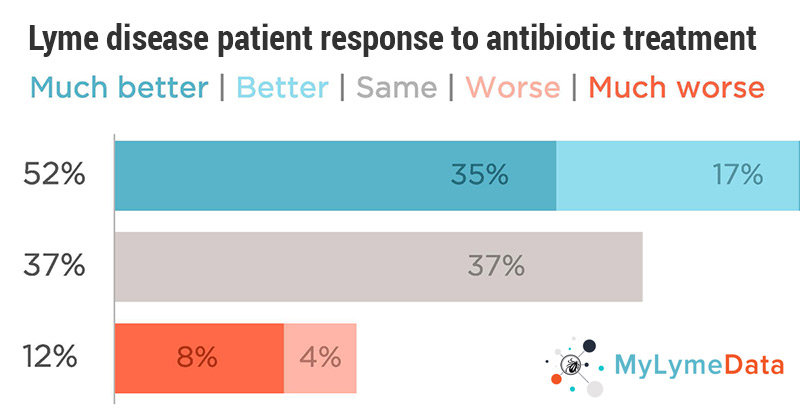
Lorraine Johnson: When we've gone out with MyLymeData and looked at patients and said, "What's worked for you?" The response is 35%, roughly a third, are getting better with antibiotic treatment. Now, that means a lot of people aren't getting better and we need better treatments. And in HIV/AIDS, they have combination treatments that are being used, we haven't even started exploring that in Lyme disease. And what happens is, when people try a treatment and it doesn't work, people will not just sit by idly and watch their lives go by. They will intervene, they will try something, and some of these other things are more risky and some of them don't work. So for example, stem cell therapy, we ask our patients, "How many of you have tried stem cell therapy?" We had 300 people in our survey, that's kind of a lot of people, who had tried stem cell survey, but only 3% said it was effective.
Charles Seales: How does this get hammered out, and is it a public relations thing, is it a medical thing?
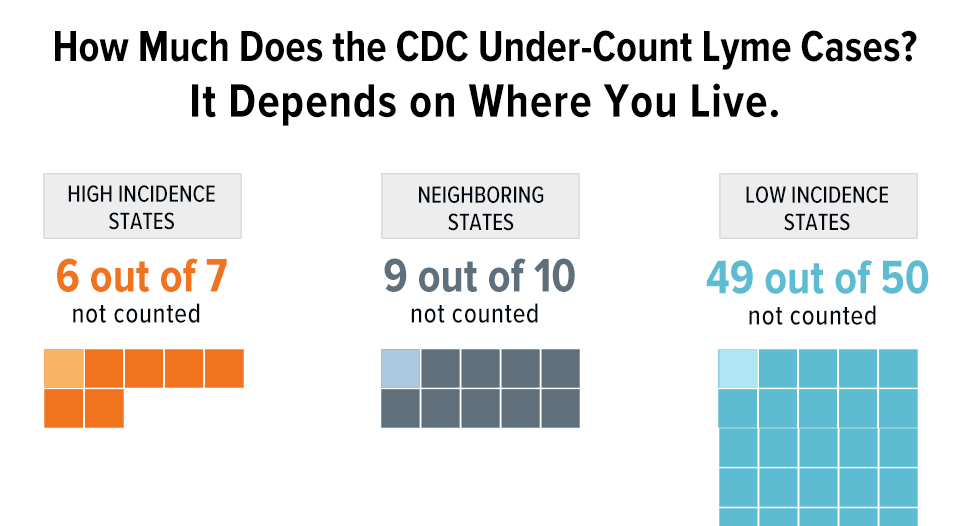
Lorraine Johnson: Well, I think it's a real combination. It's an awareness thing, so people like Yolanda speaking out, people like Avril speaking out. These are very big things because they heighten awareness, but it's also about, big data is playing a really large role in this. So when the CDC came out and said, "It's not 30,000 cases, it's 300,000 cases," they used three big data studies to do that. Quest Diagnostics came out and said, "California, the CDC reports 90 cases, but we have 4000 cases." You start to look at different data points and see how large the problem is, but I think a lot of people are leaning in right now. So you have the laboratories leaning in, some of the insurance companies are opening up their databases.
Lyme disease patient response to antibiotic treatment
MyLymeData surveyed patients and asked, “What worked for you?” The response is 35%, roughly a third, are getting better with antibiotic treatment. Now, that means a lot of people aren’t getting better and we need better treatments.
Click here for more information about MyLymeData.
Click here for more information about chronic Lyme disease.
If you are a patient who is not enrolled in MyLymeData, please enroll today. If you are a researcher who wants to collaborate with us, please contact me directly.
The MyLymeData Viz Blog is written by Lorraine Johnson, JD, MBA, who is the Chief Executive Officer of LymeDisease.org. You can contact her at lbjohnson@lymedisease.org. On Twitter, follow her @lymepolicywonk.