My presentation to the Society to Improve Diagnosis in Medicine on Lyme disease misdiagnosis.
On November 3, I was honored to give a presentation at the Patient Summit of the Society to Improve Diagnosis in Medicine’s (SIDM) annual Diagnostic Errors in Medicine (DEM) conference.
This nonprofit organization seeks to integrate and engage patients and family members in all diagnostic improvement efforts, including research, to reduce diagnostic delays and avoid missed diagnosis.
LymeDisease.org is a patient partner with SIDM’s Patients Improving Research in Diagnosis (PAIRED) project. We value the opportunity to work with this group to amplify patient concerns about how Lyme disease misdiagnosis and delays in diagnosis harm patients.
Factors that contribute to Lyme disease misdiagnosis and delays in diagnosis
My speech—which draws on insights from the MyLymeData patient registry—highlights some of the factors that contribute to delayed diagnosis or Lyme disease misdiagnosis.
We know that early diagnosis in Lyme disease can spell the difference between patients who get well quickly and are able to get on with their lives, and those who remain ill or whose course of treatment is much more difficult.
View my video presentation on Lyme disease misdiagnosis.
Lorraine Johnson: Hello. My name is Lorraine Johnson and I'm the CEO of LymeDisease.org and the principal investigator on the MyLymeData patient registry. Today I'm going to share with you a speech that I was honored to give recently to the society to improve diagnosis and medicine, a non-profit organization that seeks to bring together researchers and patients to reduce diagnostic delays and avoid Lyme disease misdiagnosis. In Lyme disease, most patients with late or chronic Lyme disease were either misdiagnosed or waited years for their diagnosis with devastating consequences. And we know that early diagnosis in Lyme disease can spell the difference between patients who get well quickly and are able to get on with their lives and those who remain ill or whose current course of treatment is much more difficult.
My speech is about some of the problems of delayed diagnosis in Lyme disease. So I wanna talk about my personal journey as a patient who's diagnosed, was missed, or delayed and how that led to the first patient-driven Lyme disease registry in the nation. So I was diagnosed with Lyme disease in 2002, but I had been sick for a long time before I was diagnosed, passed from doctor to doctor, misdiagnosed me first with MS then arthritis then gastrointestinal issues and depression, and I had all of these symptoms, sure, but they had a single cause that nobody was looking for.
And here's the thing, Lyme disease is a bacterial infection transmitted through the bite of a tick. It is treated with antibiotics and early treatment within the first month is usually effective. But by the time I was diagnosed, I had late Lyme disease, which is infinitely more difficult to treat. And without treating the underlying infection, my illness had progressed until I could no longer work or participate in family or social activities. So, Lyme disease patients often say Lyme does not kill you, it just makes you wish you were dead. It literally destroys your quality of life. And meanwhile, the antidepressants for my misdiagnosis not only did not do the job, they cause me to gain 50 unnecessary pounds. And as I thought about all of the reasons for my delayed diagnosis, and there were a lot of them, it was clear to me where I lived was a huge factor.
So Lyme disease is regarded as being primarily an East Coast disease. And here I was in California. Lyme disease was not even on the radar of my physician, so I thought, "What if, what if my physicians had recognized that Lyme disease existed in California and considered this diagnosis at my first visit." And to me it seemed like we simply needed to raise awareness of the problem, you know, identify the research, educate the physicians, and voila! Problem solved. But as it turned out, it was not so easy.
So the research base that I expected to find unfortunately didn't exist. And this chart shows how little research in Lyme disease has been done. It's from an article by Goswami and he compares a number of clinical trials conducted in different infectious diseases. And what you see here is this enormous research gap between Lyme and other infectious diseases. So let me put this in context. The CDC estimates that there are over 300,000 cases of Lyme disease each year, and that's eight times the number of new HIV/AIDS cases each year. While HIV/AIDS is at the top of the chart for the most researched studies, Lyme disease trails behind leprosy, which if you know... If you google leprosy, one commonly asked question is, does it exist in the US any longer? And it does, but there are only 200 new cases a year. So really just no comparison to the 300,000 cases of Lyme disease.
And the last clinical trial in late chronic Lyme disease was funded over 15 years ago, and there is no clinical research in the pipeline. So no one was even trying to answer the most basic questions like how many patients with later chronic Lyme disease were not diagnosed early when treatments work the best or why is their diagnosis delayed? And the bottom line is that Lyme disease is like a rare disease in terms of research. But what can patients do? Well, I can tell you what they can't do. They can't just hold tight and wait. This is a disease that takes away your very reason for living.
So this Twitter exchange, which was started by Harlan Krumholz, who until recently sat on the board of governors at the Patient-Centered Outcomes Research Institute, pretty much captures our thinking. Can we empower patients to take action and not wait on academic centers? And that's what we did. We started collecting data from patients using large-scale surveys and worked with academics to publish the results in peer-reviewed literature and it was a first time that Lyme disease patients were asked directly about delays in diagnosis, misdiagnosis, and barriers to care. And patients loved us because we asked and because it was something they could actually do.
We had thousands of patients responding and we shared with them our results as we went along. And because we were patients ourselves, we knew what questions they could answer and which ones they couldn't. So we ask them what they knew best because as Shelly's tweet here points out, for patients the mantra is "I am the gold standard of me." They know their symptoms, how long they were ill before diagnosis, what factors delayed diagnosis, and the treatments worked for them, and whether they were worth it. And then we took it a step further. In 2015, we launched the patient registry and research platform, MyLymeData, to accelerate the pace of research. And today we have over 11,000 patients enrolled throughout the country and are one of the largest patient-driven registries in the nation.
And that's what happens when patients lean in. And I wanna share with you some of the things that patients told us about delayed or misdiagnosis. So 70% of those with later chronic Lyme disease experienced years of diagnostic delays, even though 45% had early symptoms. Early diagnosis and treatment of these patients might have cured them. But it had taken the majority three or more years to be diagnosed after seeing five or more doctors. 72% were misdiagnosed and may have been unnecessarily treated for another disease like I was. So what was the problem? Why the delay? Because in Lyme disease early diagnosis, it's pretty much a ticket to recovery. 70% to 80% get well. Later on, many, many remain ill and some never recover. But a diagnosis of early Lyme disease is not straightforward. A lot of the symptoms are not specific for Lyme disease and occur in other illnesses.
So, there's a big emphasis on whether the patient has distinguishing factors. Was the patient exposed to an area where there are ticks that carry the disease? Did the patient have a distinctive round rash called an EM rash that could have been caused by the bite of a tick and were any blood test positive? And unfortunately, many of the factors used to make a diagnosis are not all that accurate, at least for those who develop late chronic Lyme disease. For example, many patients told us that they did not have a distinctive rash, only 34% did, and many about 37% had false negative lab tests. But right now, I'm just going to focus on the tick exposure question because the mere fact that I'm from California precluded my early diagnosis because no one was even looking for the disease.
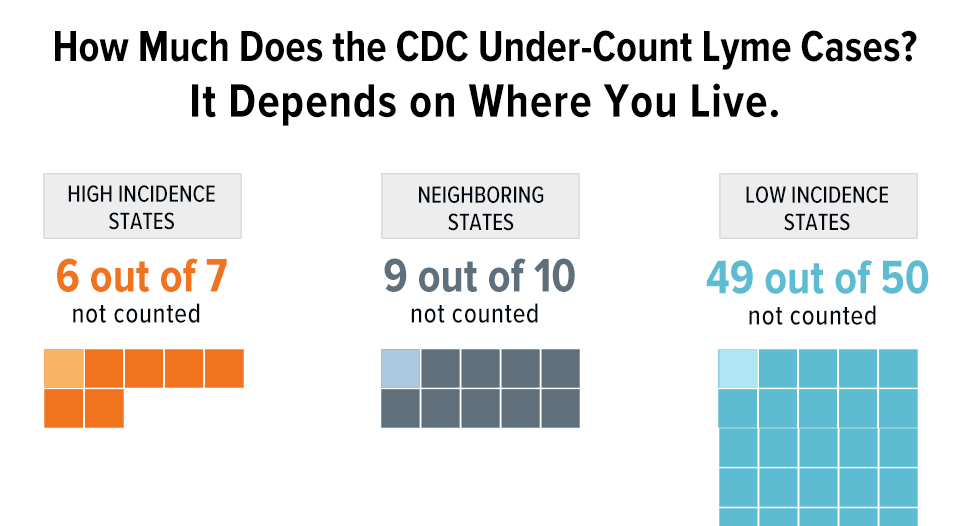
And many doctors won't test or consider Lyme disease unless the patient is from one of the top 10 states on the East Coast reflected in the Centers for Disease surveillance cases. And now one of the obvious questions that we asked was how many people outside of these top 10 states had been diagnosed with Lyme disease? And patients reported a much broader geographic reach than was reflected in the surveillance case numbers. So this map shows the geographic location of surveillance case reports compared to those in MyLymeData. And the areas in blue are the states where MyLymeData has more patients that are reported on their surveillance cases.
And as you can see, we report many more cases in the South and the West than the surveillance case report show. But for a minute, let's just consider California, where I was bitten. We showed many more patients in California, almost 800 were in our registry, but just 90 were in the surveillance cases and that's quite a gap. And bear in mind that our registry is about five times smaller than the number of surveillance case diseases. So you would always expect that the surveillance cases would outpace the reports in the registry.
And so we started to ring the bell on these differences that we were seeing. And around the same time, other data sources started confirming the California cases were in fact much higher than the surveillance numbers. So Quest Labs, for example, which is just one of seven major Labs, reported five times the number of cases reflected in surveillance data. And one of the big insurance databases, FAIR, reported close to 47,000 annual insurance claims. Now, these are claims, not cases, but still, 47,000, that's a lot of office visits, medications, and lab tests for 90 surveillance cases. And that means that California indeed has a much bigger Lyme disease problem than was previously thought.
So patient registry data helped us re-open a diagnostic question that was considered a known fact by pointing out that we do not know the true geographic reach of Lyme disease and our ability to achieve early diagnosis and successful treatment depends on getting this diagnostic threshold issue right. Early diagnosis is a winnable battle, my Lyme disease, but we can't solve it without first identifying and correcting the barriers.
And I want to close with this line, which is a bit of a celebration actually of our first publication using data from MyLymeData. It was just published two weeks ago and it is from a registry that was developed and run by patients to answer questions that patients care about. It is evidence that patients who pool their data can help drive healthcare reform and accelerate research. And I wanna thank you for giving me the opportunity to speak today.
SIDM’s PAIRED project is funded by the Patient-Centered Outcomes Research Institute and the organization has also received funding from the Agency for Healthcare Research and Quality, both of which were created by and are funded by the U.S. Congress.
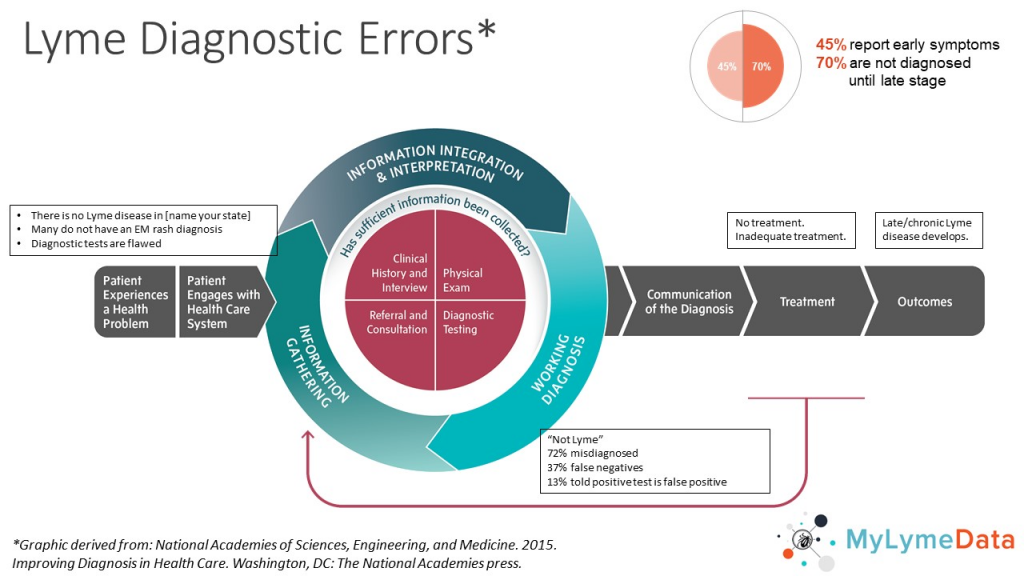
A large part of SIDM’s focus is on identifying and preventing diagnostic errors, using a diagram first developed by the Institute of Medicine (now the National Academy of Medicine) in its highly acclaimed report “Improving Diagnosis in Health Care.”
Diagnostic issues in Lyme disease
This report identifies different points along the path to diagnosis where things can go wrong and diagnosis can be delayed or missed.
We have modified the graphic from the report that illustrate points of diagnostic error to reflect the diagnostic issues we encounter in Lyme disease.
Click here to learn more about the Society to Improve Diagnosis in Medicine.
If you are a patient who is not enrolled in MyLymeData, please enroll today. If you are a researcher who wants to collaborate with us, please contact me directly.
The MyLymeData Viz Blog is written by Lorraine Johnson, JD, MBA, who is the Chief Executive Officer of LymeDisease.org. You can contact her at lbjohnson@lymedisease.org. On Twitter, follow her @lymepolicywonk.