Support for Massachusetts Insurance Legislation on Lyme disease: A Problem of Displaced Costs
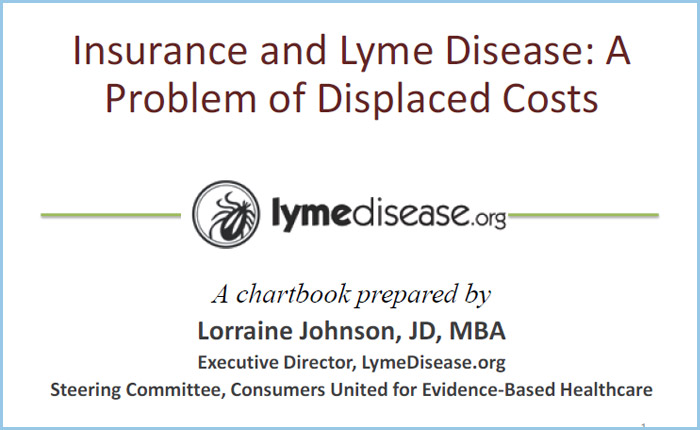
Drawing on our survey results and a key cost of illness study by Dr. Zhang of the Centers for Disease Control and Prevention, our submission in support of MA insurance legislation tells the story of how the costs of Lyme disease has been displaced by insurers onto patients, their families, society and public governments. This is particularly true in late Lyme disease, where the average annual costs exceed $20,000. Insurers bear just 12% of these costs, while patients bear the remaining 88%. Loss of productivity, when patients aren’t able to work, is the lion’s share of this—a staggering 54%.
EXCERPT OF STUDY
- direct medical costs borne by the insurer,
- indirect medical costs borne by the patient such as co-payments,
- non-medical cost like those incurred for a caretaker in the home,
- and loss of productivity costs, which principally relate to lost wages.
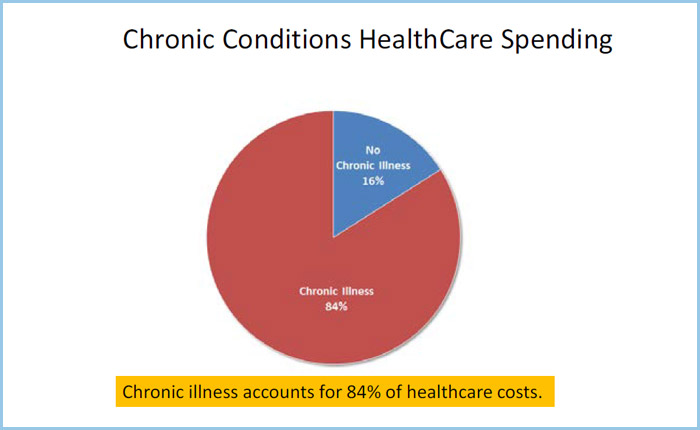
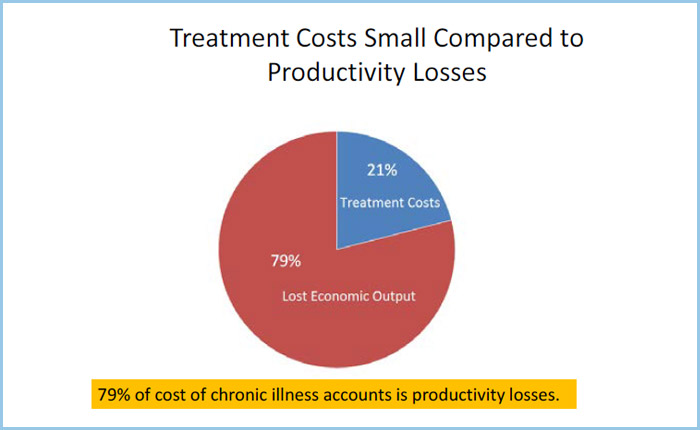
It is estimated that 79% of the cost of all chronic illness is from lost economic output of employees and only 21% of the cost is attributable to treatment costs. (Anderson 2010) This means that to reduce the total costs of the illness, we are going to get more bang for our buck—relatively speaking—by reducing loss of productivity than by reducing medical costs because that is where most of the cost is.
Insurers are only responsible for direct medical costs. Indirect medical costs like copays and the cost of loss of productivity and nonmedical costs are borne by the patient, the family, the community and ultimately the government through lost revenues from income taxes when people can’t work, through a lower gross domestic product, and through disability support payments paid by governments to those disabled by a disease. It is easy to cut medical costs, but if we increase loss of productivity in the process—then we’re simply shifting the burden of the disease from insurers to society—and we may actually increase the total costs as will be discussed later.