Is autism epidemic fueled by Bartonella and other vector-borne infections?

By Debbie Kimberg
Autism rates have been steadily rising, with more children receiving diagnoses than ever before. However, despite decades of research and millions of dollars invested in studies, there are still no clear answers about the root causes of this increase.
As a mother of a child with autism and the founder of the Autism Infectious Disease Association (AIDA), I believe one critical factor has been largely overlooked—Bartonella and other vector-borne infections may play a far greater role than currently recognized.
My journey began with my son. Diagnosed with autism at 13, he struggled with ADHD, tics, social awkwardness, ODD, OCD, PANS, and many other symptoms. But everything changed when he was finally tested for vector-borne infections—Bartonella, Babesia, and Borrelia (Lyme disease)—and the results came back positive.
After years of trial and error with treatments, he started a new approach at 16 that led to a breakthrough. More than 20 of his symptoms improved—he became more social, happy, gained 30 pounds, and excelled in school without support. It was a transformation I’d never thought possible.
Most of these improvements came after treating borreliosis and babesiosis with disulfiram, but ultimately, Bartonellosis emerged as the primary driver of his symptoms. The other infections contributed, but Bartonella played the biggest role. [1]
We are not alone in this discovery. Prominent doctors—Dr. Robert Bransfield, Dr. Kenneth Bock, Dr. Nancy O’Hara, and Dr. Rosalie Greenberg—have documented similar cases in their research, articles, interviews, and books.
I am also part of Facebook groups with thousands of other parents who have been on the same journey – with varying levels of success. This raises an urgent question: What if these infections are a hidden driver behind many cases of autism?
Understanding the Overlooked Connection: Autism and Bartonellosis
Functional medicine specialists trained in vector-borne infections have reported thousands of autism cases linked to Bartonella and similar pathogens, with many children improving after treatment. Yet, despite their findings and widespread parent testimony, this connection remains largely ignored.
Why? Because the NIH and most doctors view these infections as rare, acute illnesses, like Bartonella’s association with “cat scratch fever.” But the reality is far more complex.
These infections are likely much more common than we realize due to inaccurate testing, lack of screening, and their ability to act as stealth pathogens. These microbes can hide deep within tissues, evading the immune system, and causing chronic, wide-ranging symptoms.
For three decades, research has focused on genetic and environmental factors, along with the microbiome, yet families are still waiting for answers. Despite millions of dollars and countless studies, there is no clear explanation for why autism rates continue to climb, reaching epidemic levels.
It’s time to re-examine the basics–to investigate the role of infections like Bartonella, Babesia, and Borrelia which can penetrate the brain, disrupt immune function, and trigger chronic life-altering symptoms. The evidence is already here, waiting to be acknowledged.
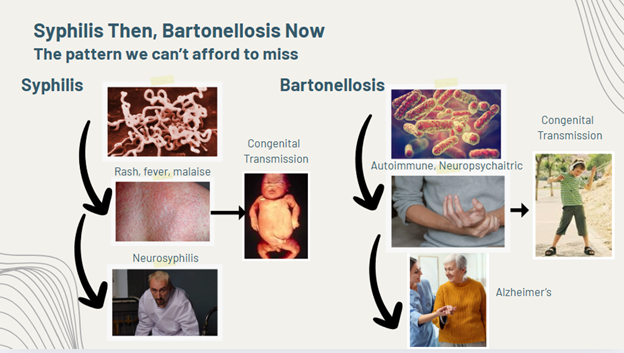
A Historical Lesson: Syphilis Then, Bartonellosis Now
History has shown us the danger of missing an infectious cause of neurological disease. Consider syphilis – an infection once thought to only cause rashes and fever. It took centuries for doctors to understand that syphilis could be passed from mother to child, causing serious malformations and neuropsychiatric symptoms.
Both syphilis and bartonellosis can cause neuropsychiatric symptoms later in life — neurosyphilis in one case and potentially Alzheimer’s in the other. While Borrelia has been detected in the brains of Alzheimer’s patients, Bartonella is also suspected to play a significant role, but requires further research to confirm its impact.
Research supports the suspicion that individuals with autoimmune diseases closely linked to bartonellosis have a higher rate of Alzheimer’s. In addition, both Borrelia and Bartonella are known to trigger chronic neuroinflammation, disrupt the blood-brain barrier, and evade the immune system, mechanisms that are also seen in Alzheimer’s pathology. [2], [3], [4]
The NIH recognizes the critical importance of preventing congenital transmission for the health of the child. Syphilis screening during pregnancy has been recommended since the 1930s. However, in the 1980s, those guidelines were strengthened to call for screening three times during pregnancy.
Are we repeating past mistakes by failing to recognize that bartonellosis may follow a similar disease progression?
A Web of Overlapping Clues
If the idea that an infection could drive autism still sounds far-fetched, consider this:
- High Rates of Autoimmunity in Autism Families: Families of autistic children have unusually high rates of autoimmune diseases (up to 70%) such as arthritis, lupus, thyroid disorders, fibromyalgia, MS, and diabetes, the very conditions that Bartonellosis is known to cause or mimic. [5], [6], [7], [8], [9], [10]
- Congenital Transmission: Bartonella is known to be passed from mother to offspring in animals like cats and mice. Clinical evidence suggests it could also be passed on to human babies, though it remains understudied. [11], [12]
- Seizures in Autism: 25–40% of autistic children experience seizures. Bartonellosis can also cause seizures, as shown in a recent case report where Bartonella DNA was found in a child’s brain tissue following seizure onset. [13], [14]
- Common Symptoms Overlap: Autism symptoms such as ADHD, gut issues, OCD, anxiety, rages, and sleep disturbances are also common symptoms of Bartonellosis. [15]
- Flare After Immune Challenge: Bartonellosis symptoms can flare after immune challenges, such as vaccines, illnesses, or even COVID. This is not unique to Bartonella. Think of chickenpox: the virus can lie dormant for decades, only to reactivate as shingles later in life, after stress or illness. Similarly, Bartonella can remain hidden in the body, emerging under immune stress.
The Taboo Vaccine Debate
This brings us to the sensitive and widely debated topic of vaccines. In autism support groups, countless parents share a strikingly similar story: their child developed normally until receiving a vaccine–often around 18 months—when autism symptoms appeared suddenly.
These are not just anecdotal accounts from strangers. Even our first doctor, along with other well-educated, science-based individuals I’ve met, experienced the same issue with their own child. These parents deserve to be heard.
Case reports have documented the reactivation of Bartonella and Herpesvirus (HHV) following COVID-19 infection. In my own family, two individuals experienced a flare of bartonellosis symptoms after receiving the COVID vaccine. Meanwhile, my asymptomatic son had new onset of bartonellosis symptoms including brain fog, exercise resistance, food sensitivities, and mild POTS, after COVID-19 infection, leading to what’s now referred to as long COVID. Some of the people who developed Long COVID after the COVID vaccine may be the first adults to experience debilitating bartonellosis symptoms triggered by a vaccine. [16], [17], [18], [19], [20]
Many long COVID symptoms seem tied to bartonellosis, much more so than to Lyme: EDS, POTS, exercise resistance, digestive symptoms, muscle and joint pain, brain fog, chronic fatigue, and sleep issues. [15]
Additionally, research has shown that many long COVID patients exhibit high antibody titers despite experiencing a wide range of persistent symptoms unrelated to acute COVID.
This pattern closely resembles what Dr. Susan Swedo identified in 1998 with PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections) where children developed sudden, disconnected neuropsychiatric symptoms following a strep infection.
The current PANDAS/PANS screening protocol includes tests for titers of strep, mycoplasma, HHV, flu A and B, coxsackie, EBV, and more. Long COVID could eventually be added to this list. Given how many children with PANDAS/PANS later test positive for Bartonella and other vector-borne infections, along with the clear overlap in neuropsychiatric symptoms, it seems only logical that screening for these infections with a high quality test from a specialty lab should become standard practice for all PANDAS/PANS diagnoses. [20], [21], [22]
My autistic son had very high strep and coxsackie titers despite never having shown any signs of those infections. Direct treatment with antibiotics and antivirals made little difference in titers and no difference in symptoms.
Immune Dysfunction?
It wasn’t until bartonellosis was treated that my son’s titers returned to normal and his symptoms significantly improved. The high titers appeared to be due to immune dysfunction, and not to the infection related to the high test titer itself. Could long COVID, PANDAS, and PANS all have the same underlying cause of latent vector-borne disease?
Regarding autism, my hypothesis is that, in some children, dormant infections—bartonellosis, babesiosis, and borreliosis—are passed from mother to child during pregnancy and remain inactive in the brain. When the child receives vaccines that stimulate the immune system, these infections may become activated, triggering the gradual or sudden onset of autism symptoms.
While these symptoms may appear to be a direct reaction to the vaccine, they could actually stem from an underlying infectious cause that had been dormant until the immune system was challenged.
If this hypothesis is proven true, the focus should not be on the danger of vaccines themselves, but rather on ensuring that mothers are free of Bartonella, Babesia, and Borrelia during pregnancy and that infants are screened at birth. This approach could prevent the onset of autism symptoms following vaccination or otherwise, providing a proactive solution rather than fueling fear.
Bartonella: The Stealth Pathogen You Need to Know About
Bartonella is not just “cat scratch fever.” It is a stealth pathogen transmitted by a wide range of vectors: ticks, fleas, lice, mites, bedbugs, and even biting spiders. It can also be transmitted through a scratch or lick on an open wound from an infected cat or dog. [23]
With up to 44% of animal workers testing positive for Bartonella, the rate in the general population may be much higher than anyone realizes. Bartonella can penetrate tissues, including the brain, heart, joints, and eyes. It also evades the immune system by hiding inside cells, biofilms, and macrophages, causing chronic illness and making it difficult to detect and even harder to treat. [24]
Standard antibody tests from commercial labs often miss these infections. Specialty labs with advanced methods like digital PCR (dPCR) provide more reliable detection. [25]
A Personal Case Study: A Family’s Journey of Discovery
In my family, the signs were all around us, but we didn’t know what to look for. My mother had OCD, anxiety, emotional lability, frequent nightmares, and night sweats. My sister struggled with anxiety, panic attacks, ADHD, dizziness (rocking floor), and in adulthood, MS and optic neuritis. I battled anxiety, a ragey temper, anorexia, suicidal ideation, and eventually suffered a still birth, thyroid disease and uveitis. One son had ODD, while another struggled with ADHD, anxiety, and eventually depression and chronic fatigue.
Eventually, three generations of our family tested positive for Bartonella, Babesia, and Lyme. Even my husband tested positive, despite being asymptomatic. What we once saw as disconnected autoimmune and neuropsychiatric symptoms were all part of the same story.
What Parents and Doctors Can Do
If you are a parent reading this, and you recognize your child and family in this story—whether your child has unexplained behaviors, neurological symptoms, ADHD, seizures, or other autism-related traits–consider the possibility of bartonellosis and other vector-borne infections. Getting screened by a functional doctor listed on ILADS.org could provide transformative insights. For support, consider joining the Facebook group, Beyond PANS: Bartonella, Lyme, MCAS, and Mold.
If you are a general practitioner who works with autistic children, please consider screening all of your patients for these underlying infections with high quality testing available through specialty labs. Treatment, while challenging, can offer life-changing results. Please contact ILADS for training information to stay on the leading edge of medicine.
A Call for Urgent Autism Research
This is not just one family’s story. It’s the reality for thousands of families navigating this journey alone, spending tens of thousands of dollars on private-pay testing and treatment because the medical system has not caught up. It is about the seven million autistic individuals who deserve to be screened for Bartonella and other vector-borne infections, the 115,000 children newly diagnosed with autism every year, and the mothers who should be screened before their child is born.
If we hope to uncover the root cause of this growing epidemic, we urgently need large-scale population studies, improved diagnostics, fast-acting cures, a broader network of trained specialists, and comprehensive insurance coverage. Families should not be forced to make these discoveries on their own and then deplete their savings to treat their sick children.
Conclusion: Will We Miss the Next Syphilis?
If we are right that congenital bartonellosis and other vector-borne infections are driving even a subset of autism cases, we have a chance to change the course of this epidemic. But achieving this will require awareness, open minds, and substantial funding for research.
This is the pattern we cannot afford to miss.
Debbie Kimberg posts about autism and Bartonella on Instagram: @hijackedbrains and on Facebook: Beyond PANS: Bartonella, Lyme, MCAS, and Mold.
Resources
Doctors: Contact ILADS at ilads.org to learn about training opportunities
Parents:
Project Lyme: Lyme Disease and Autism, an interview with Dr. Amy Offutt, Dr. Kenneth Mitchell, and Debbie Kimberg
Demystifying PANS/PANDAS: A Functional Medicine Desktop Reference on Basal Ganglia Encephalitis by Nancy O’Hara, MD.
Why Can’t I Get Better? Solving the Mystery of Lyme and Chronic Disease: Solving the Mystery of Lyme and Chronic Disease by Richard Horowitz, MD (congenital transmission)
Is There a Connection Between Autistic Spectrum Disorders and Tick-Borne Illnesses? By Rosalie Greenberg, MD
Facebook support group: Beyond PANS: Bartonella, Lyme, MCAS, and Mold
Monthly Meet Ups: Dates are posted on Mothers Against Lyme on Instagram
References
[1] Offutt, A., & Breitschwerdt, E. (2023). Case report: Substantial improvement of autism spectrum disorder in a child with learning disabilities in conjunction with treatment for poly-microbial vector borne infections. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2023.1205545
[2] Luo, W., Chen, Z., Zhang, H., Zhang, J., Lu, L., Ma, D., & Hu, Z. (2023). Increased risk of Alzheimer’s disease in patients with autoimmune diseases: A population-based retrospective cohort study. Frontiers in Immunology, 14, 1203451. https://pubmed.ncbi.nlm.nih.gov/39313029/
[3] Allen, H. B. (2021). A novel approach to the treatment and prevention of Alzheimer’s disease based on the pathology and microbiology. Journal of Alzheimer’s Disease, 84(1), 61–67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8609710/
[4] Wang, Y., Zhou, M., Meng, X., Wang, L., Huang, R., & Li, J. (2025). Autoimmune disorders are associated with an increased risk of Alzheimer’s disease: A nationwide cohort study. Cell Reports Medicine, 4(3), 100053. https://pubmed.ncbi.nlm.nih.gov/39999839/
[5] Comi, A. M., Zimmerman, A. W., Frye, V. H., Law, P. A., & Peeden, J. N. (1999). Familial clustering of autoimmune disorders and evaluation of medical risk factors in autism. Journal of Child Neurology, 14(6), 388–394. https://pubmed.ncbi.nlm.nih.gov/10385847/
[6] Atladóttir, H. Ó., Pedersen, M. G., Thorsen, P., Mortensen, P. B., Deleuran, B., Eaton, W. W., & Parner, E. T. (2009). Association of family history of autoimmune diseases and autism spectrum disorders. Pediatrics, 124(2), 687–694. https://pubmed.ncbi.nlm.nih.gov/19581261/
[7] Wu, S., Ding, Y., Wu, F., Li, R., Xie, G., Hou, J., & Mao, P. (2015). Family history of autoimmune diseases is associated with an increased risk of autism in children: A systematic review and meta-analysis. Neuroscience & Biobehavioral Reviews, 55, 322–332. https://pubmed.ncbi.nlm.nih.gov/25981892/
[8] Maggi, R. G., Pultorak, E. L., Hegarty, B. C., Bradley, J. M., Correa, M., Mozayeni, B. R., & Breitschwerdt, E. B. (2012). Bartonella spp. Bacteremia and Rheumatic Symptoms in Patients from Lyme Disease–Endemic Region. Emerging Infectious Diseases, 18(5), 783–791. https://doi.org/10.3201/eid1805.111366
[9] Aguirre-Chang, G., & Trujillo, L. (2025). The hypoxic vascular and infectious origin of rheumatic and autoimmune diseases: Chronic stiffness and pain, long COVID, MIS-C, ME/CFS, fibromyalgia, POTS, mitochondrial dysfunction, scleroderma, CREST, muscular. Unpublished manuscript. Retrieved from https://www.researchgate.net/publication/389625388
[10] Aguirre-Chang, G., & Trujillo, L. (2024). Diagnostic criteria of viral persistence for patients with long COVID, post-vaccination syndrome, MIS-C, ME/CFS, FM, MCS, arthritis, Sjögren, lupus, APS, thyroiditis, other autoimmune diseases, POTS, dysautonomia, EDS, MCAS and other diseases considered post-viral. Unpublished manuscript. Retrieved from https://www.researchgate.net/publication/376350066
[11] Siewert, L. K., Dehio, C., & Pinschewer, D. D. (2022). Adaptive immune defense prevents Bartonella persistence upon trans-placental transmission. PLOS Pathogens, 18(5), e1010453. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9113594/
[12] Tołkacz, K., Alsarraf, M., Kowalec, M., Dwużnik, D., Grzybek, M., Behnke, J. M., & Bajer, A. (2018). Bartonella infections in three species of Microtus: prevalence and genetic diversity, vertical transmission and the effect of concurrent Babesia microti infection on its success. Parasites & Vectors, 11, 491. https://parasitesandvectors.biomedcentral.com/articles/10.1186/s13071-018-3047-6
[13] Children’s Hospital of Philadelphia. (2023). Seizures and Autism Spectrum Disorder. Center for Autism Research at CHOP. https://www.research.chop.edu/car-autism-roadmap/seizures-and-autism-spectrum-disorder
[14] Breitschwerdt, E. B., & Pultorak, E. L. (2025). Bartonella henselae, Babesia odocoilei and Babesia divergens-like MO-1 infection in the brain of a child with seizures. Therapeutic Advances in Infectious Disease. https://doi.org/10.1177/11795735251322456
[15] Breitschwerdt, E. B., Bradley, J. M., Maggi, R. G., Lashnits, E., & Reicherter, P. (2020). Bartonella Associated Cutaneous Lesions (BACL) in People with Neuropsychiatric Symptoms. Pathogens, 9(12), 1023. https://www.mdpi.com/2076-0817/9/12/1023
[16] Aubry, A., Corvilain, E., Ghelfenstein-Ferreira, T., Camelena, F., Meignin, V., Berçot, B., Le Goff, J., & Salmona, M. (2024). Unmasking Bartonella henselae infection in the shadows of long COVID thanks to clinical metagenomics. European Journal of Clinical Microbiology & Infectious Diseases, 43(5), 1025-1029. https://pubmed.ncbi.nlm.nih.gov/38472519/
[17] Dong, Y., Alhaskawi, A., Zou, X., et al. (2024). Post-COVID reactivation of latent Bartonella henselae infection: A case report and literature review. BMC Infectious Diseases, 24, 422. https://pubmed.ncbi.nlm.nih.gov/38649899/
[18] Katsafadou, A. I., Vontas, A., & Tsitsakis, A. M. (2023). Reactivation of Herpesviruses Following COVID-19 Vaccination: A Systematic Review and Meta-Analysis. European Journal of Medical Research, 28(1), 38. https://pubmed.ncbi.nlm.nih.gov/37559096/
[19] Yale News. (2025, February 19). Immune markers of post-vaccination syndrome indicate future research directions. Yale News. Retrieved from https://news.yale.edu/2025/02/19/immune-markers-post-vaccination-syndrome-indicate-future-research-directions
[20] de Sá, K. S. G., Silva, J., Bayarri-Olmos, R., Brinda, R., Constable, R. A. R., Colom Diaz, P. A., … & Iwasaki, A. (2024). A causal link between autoantibodies and neurological symptoms in long COVID. medRxiv. https://pubmed.ncbi.nlm.nih.gov/38947091/
[21] Swedo, S. E., Leonard, H. L., Garvey, M., Mittleman, B., Allen, A. J., Perlmutter, S., … & Rapoport, J. L. (1998). Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: Clinical description of the first 50 cases. The American Journal of Psychiatry, 155(2), 264–271. https://pubmed.ncbi.nlm.nih.gov/9464208/
[22] PANDAS Network. (2020). Basic Blood Work. Retrieved from https://pandasnetwork.org/wp-content/uploads/2020/09/BASIC-BLOOD-WORK.pdf
[23] Breitschwerdt, E. B., Maggi, R. G., Duncan, A. W., Nicholson, W. L., Hegarty, B. C., & Woods, C. W. (2007). Bartonella Species in Blood of Immunocompetent Persons with Animal and Arthropod Contact. Emerging Infectious Diseases, 13(6), 938-941. https://doi.org/10.3201/eid1306.061337
[24] LymeDisease.org. (2022). Bartonella is more prevalent in Lyme disease than previously thought. https://www.lymedisease.org/bartonella-prevalent-lyme-disease/
[25] Ericson, M. E., Mozayeni, B. R., Radovsky, L., & Bemis, L. T. (2024). Bartonella- and Borrelia-Related Disease Presenting as a Neurological Condition Revealing the Need for Better Diagnostics. Microorganisms, 12(1), 209. https://doi.org/10.3390/microorganisms12010209




















We invite you to comment on our Facebook page.
Visit LymeDisease.org Facebook Page