M illions of Americans are likely to be bitten by ticks this year. Some of them may know enough to be concerned about Lyme disease. However, the public at large—and many medical professionals—are often oblivious to other dangers posed by ticks. (See my previous discussion of co-infections here.)
Some particularly troublesome bacteria belong to a group called Rickettsia. Although they can also be found in lice, fleas, mites, and chiggers, in the U.S., most rickettsial infections are thought to be transmitted by ticks.
Rickettsia includes two different groups: the spotted fever group (which consists of rickettsiae and ehrlichia) and the typhus group. This post will focus on spotted fever group rickettsiae (SFGR), which includes:
- Rickettsia rickettsii, also known as Rocky Mountain spotted fever (RMSF)
- Rickettsia parkeri
- Rickettsia philipii, (previously 364D) the cause of Pacific Coast tick fever
- Rickettsia helvetica* (which may be found in the U.S.)
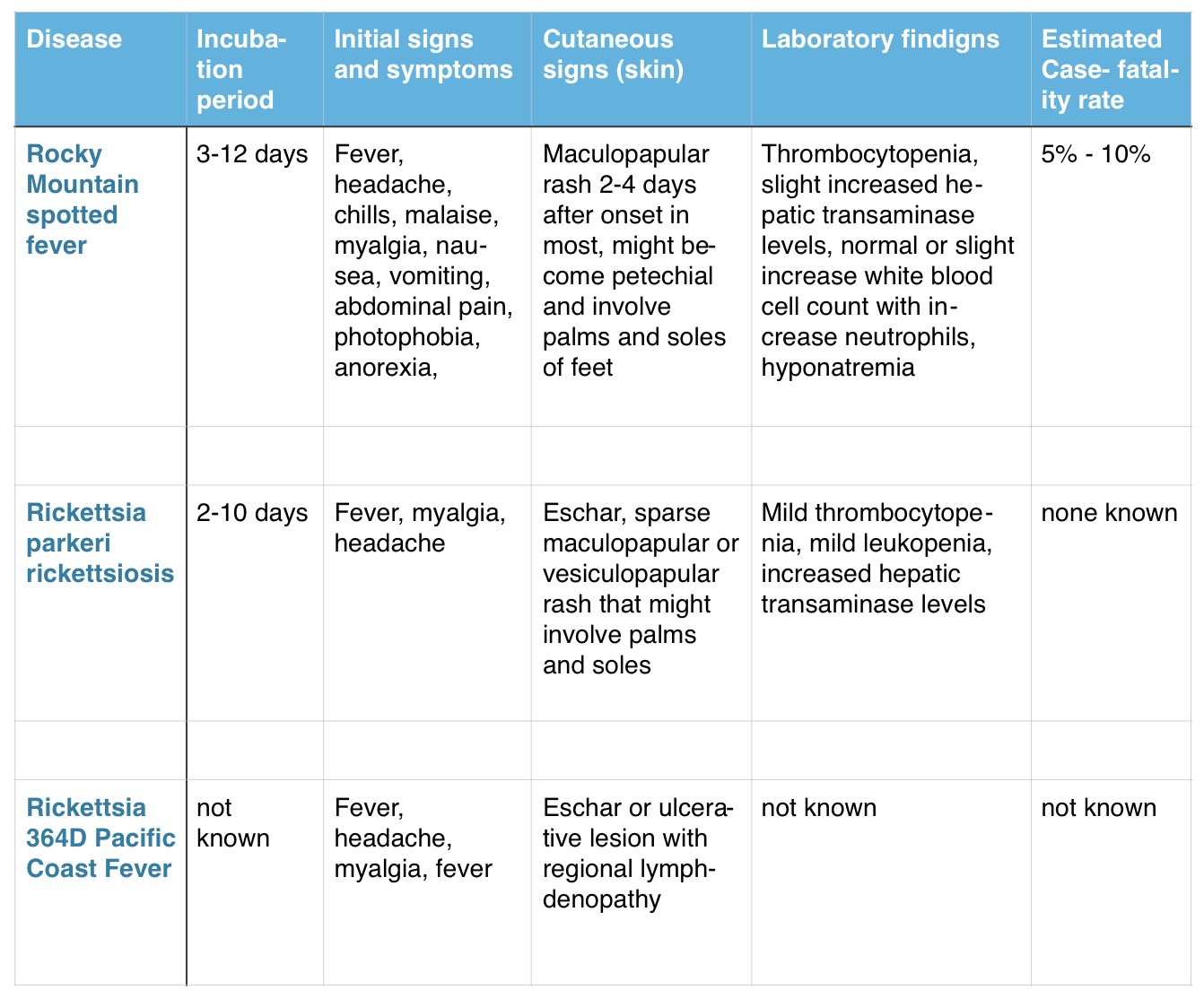
Rocky Mountain Spotted Fever
Rocky Mountain spotted fever (RMSF) is the most common rickettsial infection in the U.S. It can range from a mild illness to a fatal one.
Initial symptoms typically include high fever, severe headache, abdominal pain (with or without vomiting), and muscle pain. It often—though not always—includes a spotted rash that begins at the wrist and/or ankles, and spreads outward from there.
According to the CDC website:
“RMSF is a serious illness that can be fatal in the first eight days of symptoms if not treated correctly, even in previously healthy people. The progression of the disease varies greatly. Patients who are treated early may recover quickly on outpatient medication, while those who experience a more severe course may require intravenous antibiotics, prolonged hospitalization or intensive care.”
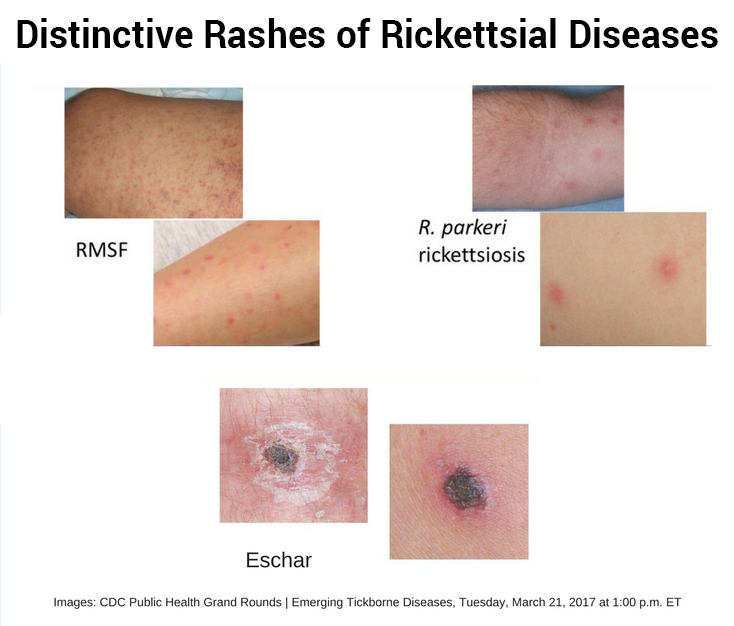
RMSF weakens small blood vessels throughout the body, giving rise to its characteristic rash. This widespread damage to the blood vessels allows the bacteria to spread to the heart and brain—and can quickly lead to death in those under age 4, over the age of 60, or those whose immune systems are compromised.
RMSF can also result in permanent nerve/organ damage or amputation. In one tragic case, an Oklahoma woman’s infection went unrecognized until it was too late. To save her life, doctors had to amputate both arms and both legs.
Prior to the use of antibiotics, RMSF had a fatality rate of up to 80%.
In the U.S. today, the fatality rate is 5%-10%. However, in neighboring Mexico, fatality rates from RMSF in recent years have been as high as 30%.
An interesting case study occurred in eastern Arizona, where there are no known American dog ticks (the primary vector of RMSF). Beginning in 2003, there were outbreaks of RMSF on several Indian reservations, with the rate of infection reaching 150 times the national average, including 19 fatalities. This was later attributed to the large population of free-roaming dogs. Unexpectedly, a different vector was identified as the culprit in these cases, the brown dog tick.
Community leaders and public health officials dramatically reduced the rate of RMSF by treating the yards of 500 homes with acaricide (pesticides that target ticks) and placing long-acting tick collars on over 1000 dogs.
Afterward, ticks were only found on 1% of the dogs with collars versus 64% of the untreated dogs. These collaborative efforts helped reduce RMSF by 43% on the reservations.
Other Types of Rickettsiosis
Rickettsia parkerii, found along the Gulf Coast, and R. phillipii, from the West Coast, cause a milder form of rickettsiosis. The spotted rash is not as common but both will frequently cause an eschar (scab) or necrotic area about one centimeter across at the site of the tick bite. These other types of Rickettsiosis usually result in a mild illness that may go undiagnosed. Thus, the actual number of infections may be higher than we know.
Transmission
In the United States, Rickettsiosis is primarily transmitted by the following ticks:
- American dog tick (Dermacentor variabilis)
- Rocky Mountain wood tick (Dermacentor andersoni)
- Brown dog tick (Rhipicephalus sanguineus)
- Gulf Coast tick (Amblyomma maculatum)
- Pacific Coast ticks (Dermacentor occidentalis)
Distribution
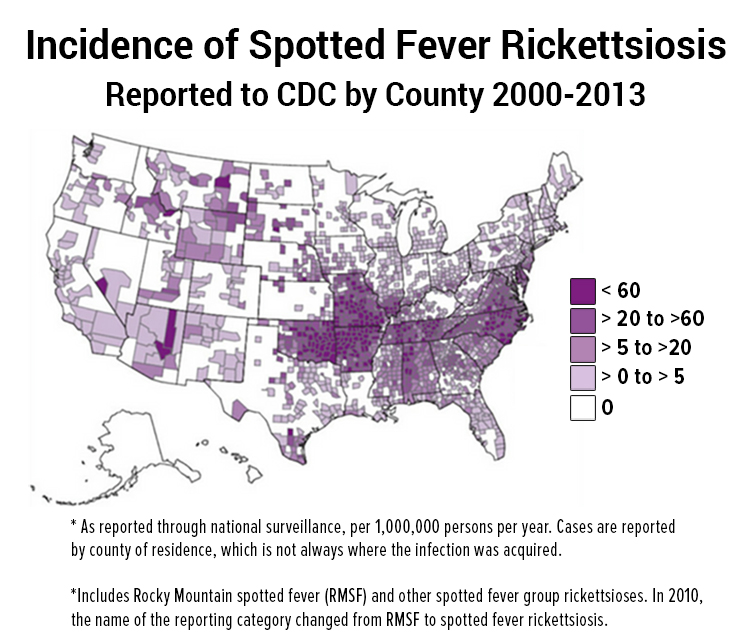
According to the CDC, rickettsial diseases have been reported in every state except Alaska and Hawaii. In those two states, officials are not required to keep track of rickettsial diseases, so nobody knows how many cases may be there.
Incidence
In 2009, the reporting definition for RMSF was changed to include the more broad “Spotted Fever Rickettsiosis” (SFR) which includes RMSF. Using the new criteria, there were 4470 reported cases of spotted fever rickettsiosis in 2012, the majority of which were presumed to be RMSF. In general, the number of cases of SFR are increasing–from 1.7 cases per million in 2000 to an all-time high of 14.2 cases per million in 2012.
Risk Factors
People who spend time outdoors, American Indians who live on reservations, and dog owners are at higher risk for contracting rickettsiosis. In a large survey conducted by LymeDisease.org, 26% of respondents reported having a rickettsial co-infection, with 6% having RMSF.
Conclusion
If you’ve been exposed to ticks and come down with a flu-like illness, be aware that you may have been infected with a tick-borne disease separate from or in addition to Lyme disease. Mainstream doctors typically do not test for co-infections. Knowing the signs and making your physician aware of the appropriate treatment for SFGR may save your life or that of a loved one.
Summary of Spotted Fever Rickettsiosis Found in U.S.
*Rickettsia helvetica was discovered by Dr. Willy Burgdorfer in 1978 and widely thought to be found only in Europe. However, it was recently uncovered in Burgdorfer’s 35-year-old archives that he had seen a bacterium that highly resembled R. helvetica inside the samples of blood containing Borrelia (the bacteria that causes Lyme disease). He called this microbe the “Swiss Agent.” (You can read more about that discovery here.)
LymeSci is written by Lonnie Marcum, a licensed physical therapist and mother of a daughter with Lyme. Follow her on Twitter: @LonnieRhea Email her at: lmarcum@lymedisease.org.