Treating Bartonella-Like Organisms There may be as many as 30 distinct pathogenic species of Bartonella-like organisms, most of which have never been clinically defined.
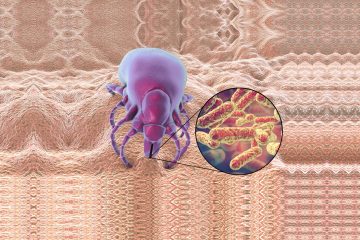
I t has been said that Bartonella is the most common of all tick-borne pathogens. Indeed, there seems to be a fairly distinct clinical syndrome when this type of organism is present in the chronic Lyme patient. However, several aspects of this infection seem to indicate that these tick-associated strains of Bartonella are different from that described as “cat scratch disease.”
For example, in patients who fit the clinical picture, standard Bartonella blood testing is commonly non-reactive.
Furthermore, the usual Bartonella medications do not work for this–they suppress the symptoms but do not permanently clear them. Recently, thanks to advanced genotyping, it has been discovered that there may be as many as 30 distinct pathogenic species of this organism, most of which have never been clinically defined, and drug treatment studies, if they exist at all, are often misleading because for this intracellular organism, in vitro results rarely reflect in vivo efficacy. For these reasons, I like to refer to this group collectively as “Bartonella-like organisms” (BLOs).
Indicators of BLO infection include symptoms involving the central nervous system (CNS) that are out of proportion to the other systemic symptoms of disseminated Lyme disease.
There seems to be an increased irritability to the CNS, with agitation, anxiety, insomnia, twitches, tremors, and even seizures, plus symptoms of encephalitis, such as cognitive deficits and confusion. In addition, aggressive, antisocial, and inappropriate behavior has been observed, especially in young adults.
Other key symptoms may include ocular inflammation, gastritis, lower abdominal pain (mesenteric adenitis), sore soles, especially in the morning, tender subcutaneous nodules along the extensor tendons of the extremities, and red rashes.
 These rashes may have the appearance of red streaks like stretch marks that do not follow skin planes, spider veins, and/or red papular eruptions. Lymph nodes may be enlarged and the throat can be sore. Unlike borreliosis, which often causes a low-grade fever in the afternoon and a subnormal temperature in the morning, BLO infections cause an early-morning temperature elevation, mild enough that it often is missed by the patient. Keeping temperature diaries can be very useful in this instance.
These rashes may have the appearance of red streaks like stretch marks that do not follow skin planes, spider veins, and/or red papular eruptions. Lymph nodes may be enlarged and the throat can be sore. Unlike borreliosis, which often causes a low-grade fever in the afternoon and a subnormal temperature in the morning, BLO infections cause an early-morning temperature elevation, mild enough that it often is missed by the patient. Keeping temperature diaries can be very useful in this instance.
Because standard Bartonella testing, either by serology or PCR, is very insensitive, the diagnosis is a clinical one, based on the above points. Also, suspect infection with BLOs in extensively treated Lyme patients who still are encephalitic and who never had been treated with a significant course of treatment known to be effective for BLOs.
Treating BLOs can be difficult, as drug resistance can rapidly develop to macrolides and fluoroquinolones when used as a single agent and solo courses of tetracyclines are ineffective. Cell wall drugs by themselves inhibit BLOs but do not eradicate them, but will synergize with intracellular agents. Consider adding gentamicin, as clinical studies have shown this to be essential in the most severe cases. Bottom line is that for advanced disease, as in borreliosis, drug combinations usually are needed for synergism and to decrease the risk of drug resistance.
The drug of choice to treat BLOs is levofloxacin and related advanced fluoroquinolones. Levofloxacin is usually never used for Lyme or Babesia. Thus many patients who have tick-borne diseases, who have been treated for them but remain ill may in fact be infected with BLOs. Unfortunately, levofloxacin and drugs in this family cannot be given in pregnancy or to those under the age of 18, so other alternatives, such as azithromycin and/or Rifampin, are used in these cases.
Another subtlety is that certain antibiotic combinations seem to inhibit the action of fluoroquinolones, while others seem to be neutral or additive. I advise against combining a fluoroquinolone with an erythromycin-like drug, as clinically such patients do poorly. On the other hand, combinations with cephalosporins and penicillins enhance recovery. Alternatives to levofloxacin include combinations that include Rifampin, azithromycin, gentamicin, and possibly streptomycin.
Treat for at least one month, and four months or longer is often needed for the more ill patients.
Complimentary therapies are frequently added to the treatment regimen. Supplemental arginine can reverse the epigenetic changes in the host that are caused by BLO infection, and transfer factors specific to this infection appear to be clinically helpful.
Incidentally, animal studies show that Bartonella may be transmitted across the placenta in some species, and in humans, a single case report did outline suspected maternal-fetal transmission of both B. henselae and B. vinsonii subsp. berkoffii.
Editor’s note: Any medical information included is based on personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.