“Lyme Complex” Triggers Pandemonium in Immune System Dr. Daniel Kinderlehrer's book, "Recovery from Lyme Disease: The Integrative Medicine Guide to Diagnosing and Treating Tick-Borne Illness" discusses how this happens.
I n 1996, Dr. Daniel Kinderlehrer had practiced integrative medicine for seventeen years, focusing heavily on food sensitivities, digestive issues, and nutritional supplementation.

Then, he suddenly developed a serious illness himself. It started with fever, chills, and muscle aches, which waxed and waned with alarming frequency. Eventually, this ailment would spin his life and medical practice into an entirely new direction.
During Kinderlehrer’s initial search for what was wrong, he tested positive for Lyme disease. At first, that diagnosis brought relief. The standard medical advice was that a short course of antibiotics would clear the infection. Soon, he thought, he’d be good to go.
Uh-oh. That’s not how things turned out.
“The Lab Must Be Wrong”
Kinderlehrer started the suggested treatment and promptly got worse. Intractable insomnia, anxiety, violent shaking of his body. Finally, he contacted a prominent physician with a reputation as an expert in Lyme disease.
“You don’t have Lyme,” [the expert] concluded.
“Well, then, what do I have?” I was confused.
“Something else,” he replied.
“But what about the lab tests?” I asked. “Using the western blot technique, the assay demonstrated the presence of antibodies highly specific for Lyme. I even repeated the tests one month later, and they confirmed the initial results. Isn’t this the CDC criteria for the diagnosis of Lyme?”
“The laboratory must have been wrong,” he informed me.
“Why do you think I don’t have Lyme?” I responded.
“Because if you had Lyme, you’d be better by now.”
(Many people with persistent Lyme symptoms report being told something similar by doctors. I well recall the infectious disease “expert” my own family consulted early on in my daughter’s illness. This prominent member of the Infectious Diseases Society of America stated point-blank that since she had completed thirty days of antibiotics with no change in symptoms, that “proved” she didn’t have Lyme disease.)
New Book
At that point, Kinderlehrer set out to find answers for himself. In time, what he learned would be shared with hundreds of patients who eventually flocked to his practice, which now focuses entirely on tick-borne infections. And it led to a new book, Recovery from Lyme Disease: The Integrative Medicine Guide to Diagnosing and Treating Tick-Borne Illness.
Recovery from Lyme Disease has twenty-five chapters, divided into five sections:
 Anatomy Lessons: Anatomy of an illness, an epidemic, and the Lyme wars
Anatomy Lessons: Anatomy of an illness, an epidemic, and the Lyme wars
 Meet the Bugs” Explanation of the different microbes involved with what Kinderlehrer calls “Lyme disease complex,” in which the Lyme bacterium, Borrelia burgdorferi, plays only one part
Meet the Bugs” Explanation of the different microbes involved with what Kinderlehrer calls “Lyme disease complex,” in which the Lyme bacterium, Borrelia burgdorferi, plays only one part
 It’s all Connected: Endocrine dysfunction, gastrointestinal issues, nervous system disorders, inflammation, detoxification, fatigue, diet and nutrition
It’s all Connected: Endocrine dysfunction, gastrointestinal issues, nervous system disorders, inflammation, detoxification, fatigue, diet and nutrition
 What Else? Other considerations, alternative treatments, frequently asked questions
What Else? Other considerations, alternative treatments, frequently asked questions
 The Challenge: Discussion of what it will take to get us where we want to go; appendices; acknowledgements
The Challenge: Discussion of what it will take to get us where we want to go; appendices; acknowledgements
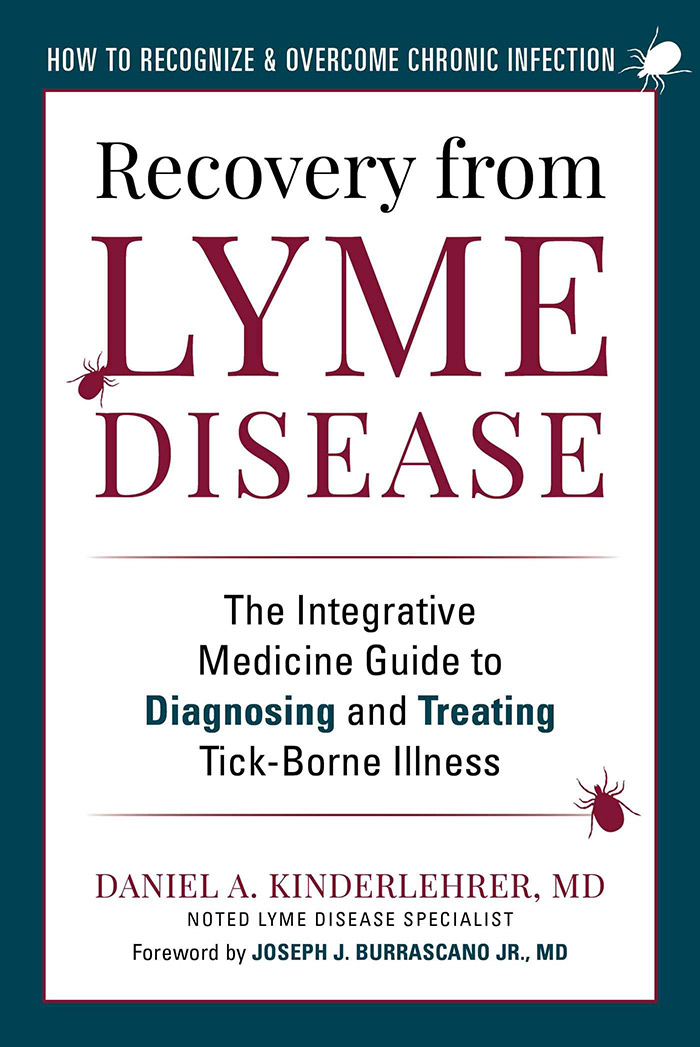
Chapter 18 (in Section 3) includes an excellent description of the immune system—particularly germane to COVID as well as to Lyme disease complex.
As the author puts it, “Lyme and its co-infections trigger pandemonium in the immune system, resulting in excessive systemic inflammation and auto-immunity as well as immune suppression. A multisystemic approach is necessary to control inflammation: avoiding allergic triggers, healing the gut, balancing hormones, calming the nervous system, enhancing detoxification—as well as treating infections.”
Kinderlehrer gives good explanations of tests, treatments, and alternative approaches to dealing with these issues.
Author: Dr. Daniel Kinderlehrer
In Recovery from Lyme Disease, Dr. Kinderlehrer gives good explanations of tests, treatments, and alternative approaches to dealing with the pandemonium in the immune system that Lyme and its co-infections trigger.
An excerpt from Dr. Daniel Kinderlehrer’s book
Recovery from Lyme Disease
The following is an excerpt of “Recovery from Lyme Disease: The Integrative Medicine Guide to Diagnosing and Treating Tick-Borne Illness.”
Sometimes there is a moment in a person’s life that, although seemingly insignificant at the time, heralds a drastic and unalterable change in everything that follows. For me, it was August 15, 1996.
The “insignificant event” was, I thought, a virus. I had a fever and chills. The fever was high, 104 degrees, and the chills made my teeth chatter and the bed shake. My body ached so much I felt like a discarded New England Patriot’s tackling dummy.
But I had no other symptoms commonly associated with the flu, no cough or respiratory congestion, and influenza does not occur in the summer. I didn’t have the upset stomach or diarrhea typical of a stomach bug, either. I never saw an insect bite, and I didn’t notice a rash. For two days I was so sick I stopped worrying I would die, and started fearing that I would live. On the third day, it was all just a memory.
It seemed quite strange, but since I was able to resume full activity, including several three-mile runs, I didn’t think much of it—until one week later, when it hit again. Once more, the fever, chills, and muscle aches lasted two days and then went away. Still pretty strange, I thought, but since I felt well after this relapse I chose to ignore it.
Denial works well when you feel okay. But when the symptoms recurred for the third time a week later, the denial stopped working and I began to worry. This time I went to see a physician friend of mine. Upon examination, he palpated an enlarged spleen. He ordered some blood tests, and the laboratory reported a positive antibody test to Lyme. The diagnosis came as a relief. The cause of my problems was a simple bacterial infection. Two weeks of antibiotics would clear it, and then I could resume my normal life.
Was I in for a Surprise!
 I tolerated the antibiotics without difficulty, and the fever and chills did not return. But instead of feeling better, I felt worse. The next symptom that hit me, and hit me hard, was insomnia. One night I woke up at 4:00 a.m., and couldn’t fall back to sleep. The next night I woke up at 3:00 a.m., the next at 2:00 a.m., and then 1:00 a.m., unable to go back to sleep. This went on for weeks. I only slept a few hours a night. I was exhausted. But even worse, I became consumed with anxiety.
I tolerated the antibiotics without difficulty, and the fever and chills did not return. But instead of feeling better, I felt worse. The next symptom that hit me, and hit me hard, was insomnia. One night I woke up at 4:00 a.m., and couldn’t fall back to sleep. The next night I woke up at 3:00 a.m., the next at 2:00 a.m., and then 1:00 a.m., unable to go back to sleep. This went on for weeks. I only slept a few hours a night. I was exhausted. But even worse, I became consumed with anxiety.
I would lie awake through the dark hours of the night riddled with fear. Initially the apprehension focused on my sleeplessness, anticipating the difficulty of getting through the day in my worn-out state. Gradually the anxiety generalized into a constant dread that something terrible was about to happen—impending doom.
It wasn’t rational. It wasn’t something I could control with reason. It was just always there. It felt like a black cloud was enveloping me, cutting me off from any future. It was pure existential terror. It was so intense that some nights, as I lay awake with insomnia, I shook so violently that I added disrupting the San Andreas fault to my list of fears—and I was living in Boston!
Although I’m a physician, I had little experience with Lyme. So I mustered what energy I could—I phoned a Lyme specialist in Boston at the Tufts-New England Medical Center, my alma mater, who was considered a world expert in Lyme disease and asked for advice. He listened courteously to my story as I described my history of symptoms and lab tests, but what he told me came as a shock.
You don’t have Lyme,” [the expert] concluded.
Well, then, what do I have?” I was confused.
Something else,” he replied.
But what about the lab tests?” I asked. “Using the western blot technique, the assay demonstrated the presence of antibodies highly specific for Lyme. I even repeated the tests one month later, and they confirmed the initial results. Isn’t this the CDC criteria for the diagnosis of Lyme?”
The laboratory must have been wrong,” he informed me.
Why do you think I don’t have Lyme?” I responded.
Because if you had Lyme, you’d be better by now.”
My First Taste of Controversy
I thanked him for his time, hung up the phone, and tried to make sense out of what I had just heard. I considered this doctor’s logic: if the cure didn’t work, I didn’t have the disease. I had had an acute illness with fever, chills, and muscle aches. I had blood tests that confirmed a diagnosis of Lyme. I lived in an area endemic for Lyme. I had seen deer ticks on our dog. I continued to feel terrible, but I didn’t have Lyme because I wasn’t better. I was getting my first taste of the controversies surrounding Lyme disease.
 Next I consulted with a friend and colleague, a physician in upstate New York who treats a lot of people with Lyme. When I told him what the Lyme expert had said he replied, “Welcome to the Lyme wars.”
Next I consulted with a friend and colleague, a physician in upstate New York who treats a lot of people with Lyme. When I told him what the Lyme expert had said he replied, “Welcome to the Lyme wars.”
He informed me that there are two different Lyme camps: those who maintain that Lyme is hard to get and easy to treat, and those who believe Lyme is easy to get and hard to treat. The so-called Lyme expert was a strong proponent to the former. Given my personal experience, I now subscribed to the latter.
What is clear now is that while the Lyme expert was categorically wrong when he denied I had Lyme, he was correct that I did indeed have “something else.” The something else was a co-infection, specifically Babesia. However, this bug was under the radar in 1996. If I were taking my history now, I would immediately suspect this infection.
I have shared my story here because there are millions of people today suffering as I did: people who are losing their cognitive function, are severely depressed, anxious and irritable, in chronic pain, and tired beyond exhaustion; people who are losing their jobs, are disabled, are going bankrupt, and whose families are breaking up; people who are contemplating suicide—and sometimes following through. The toll in medical costs and lost income is huge. The toll in human suffering is beyond calculation.
No Magic Pill
 The bad news I learned on my journey is that there is no single treatment regimen that will cure any chronic illness—no magic pill, no simple injection. Healing from chronic illness requires a multipronged and multidimensional approach. Each person is different, and treatment protocols need to be individualized. It requires assembling the pieces of a puzzle, with each person presenting his or her own clues. There is no single recipe for success.
The bad news I learned on my journey is that there is no single treatment regimen that will cure any chronic illness—no magic pill, no simple injection. Healing from chronic illness requires a multipronged and multidimensional approach. Each person is different, and treatment protocols need to be individualized. It requires assembling the pieces of a puzzle, with each person presenting his or her own clues. There is no single recipe for success.
While Lyme has been the worst thing that has ever happened to me, it has also been the best. This experience has been profoundly humbling. There were times I felt so poorly that the only way I could get through the day was to tell myself that tomorrow I could commit suicide.
But Lyme has also blessed me with deep compassion and empathy for others who are suffering. Lyme has stirred in me a passionate commitment to help others who are challenged with this illness. Lyme has filled me with hope that each and every patient coming through my office door will get well. I can’t think of anything more rewarding or more gratifying than helping people restore their well-being.
Healing from chronic illness requires a multipronged and multidimensional approach. Each person is different, and treatment protocols need to be individualized. There is no single recipe for success.
My medical practice is now limited to treating people with tick-borne infections. And despite living in Colorado, where the state Department of Health continues to deny that one can acquire Lyme disease, I have a long waiting list that keeps growing. There is a huge need out there for more Lyme literate practitioners, and I hope this book will help both physicians and patients better address this tremendous demand.
An excerpt from Dr. Daniel Kinderlehrer’s book
Recovery from Lyme Disease
I am frequently asked how I treat Lyme disease. My answer is that I don’t—I treat people, and they are all different.
There is no cookbook, even for treating early or acute Lyme disease. Ideally patients should avoid any practitioner who uses a “one size fits all” approach. Treating Lyme patients effectively is complicated. This chapter will explain why.
Issues with acute Lyme disease
Acute Lyme disease would seem to be straightforward. A recent infection should be easily diagnosed and treated. But it often isn’t.
Here’s why:
- Many people, perhaps most, do not observe a tick attachment.
- A rash is often absent, missed, or ignored.
- The early symptoms of acute Lyme disease may be absent or mild, or self-diagnosed as the flu, and therefore ignored by the patient.
- The diagnosis of acute Lyme disease is often missed by medical practitioners.
- The standard treatment recommended for acute Lyme disease is inadequate for eradicating the infection in many people.
- Infection with the Lyme bacteria is frequently accompanied by co-infections that require different antibiotics as well as more aggressive treatment.
- Some patients who present with acute Lyme are, unwittingly, suffering from chronic tick-borne infections that were acquired at some time in the past.
- Borrelia burgdorferi (Bb) can suppress the immune system, resulting in persistent infection.
- Although acute Lyme disease is characterized as being localized to the skin, Borrelia burgdorferi can spread systemically by the time the rash appears.
- The previous chapter highlighted the several ways in which Bb has evolved to evade the immune system and resist antibiotics. In addition, not all Bb bacteria are the same; there are multiple strains of Bb, each with varying degrees of virulence and an affinity for different organs.
Chronic infection is more complicated
 Chronic infection is a different ball game altogether. The majority of patients with chronic illness do not just have a long-term infestation with Bb. Rather, their Lyme disease complex* often includes other tick-borne infections, referred to as co-infections. Multiple studies have confirmed that ticks are veritable cesspools of microbes, and a single tick may harbor a handful of different bacteria.
Chronic infection is a different ball game altogether. The majority of patients with chronic illness do not just have a long-term infestation with Bb. Rather, their Lyme disease complex* often includes other tick-borne infections, referred to as co-infections. Multiple studies have confirmed that ticks are veritable cesspools of microbes, and a single tick may harbor a handful of different bacteria.
For example, a collection of 286 ticks in upstate New York revealed that 64 percent had Bb, 20 percent had Anaplasma and 20 percent had Babesia; but 17 percent had Bb and Babesia, 16 percent had Bb and Anaplasma, and 5 percent had all three. One of the ticks had four pathogens: Bb, Babesia, Anaplasma, and B.miyamotoi. In fact, co-infection of ticks is the rule rather than the exception. Dr. Joseph Burrascano refers to these ticks as “nature’s dirty needles.”
The presence of combined infections typically causes more severe symptoms than Bb by itself. The immune suppression from Bb infection is compounded by co-infections, and polymicrobial infections are more difficult to treat.
There is no cookbook, even for treating early or acute Lyme disease. Ideally patients should avoid any practitioner who uses a “one size fits all” approach.
Virtually all patients with Lyme disease complex are co-infected, and treatment of persistent infection with Bb will be unsuccessful unless therapy is also directed at these co-infections.
Many additional complications have been associated with Lyme disease complex:
- Chronic inflammation associated with chronic infection results in many imbalances throughout the body. These will be discussed in detail in subsequent chapters.
- Detoxification pathways get overloaded and fail to metabolize and excrete toxins efficiently. (See Chapter 19.)
- Adrenal glands, which work hard to compensate for the ongoing stress, lose their reserve and in time become overtaxed, resulting in adrenal insufficiency. This not only induces fatigue, but also contributes to immune dysfunction. (See Chapter 15.)
- Hypothyroidism is common—even people with normal thyroid gland function can present with symptoms of hypothyroidism. They often are converting too much of their T4 hormone to reverse T3, a form that blocks thyroid action at the cellular level, rather than making the usable form of the hormone. (See Chapter 15.)
- Insulin resistance leads to elevated insulin levels, resulting in increased inflammation, fatigue, and immune suppression. (See Chapter 15.)
- The autonomic nervous system, which regulates the body’s automatic activities such as breathing, pulse, and body temperature, becomes destabilized. The resulting dysautonomia can cause chaotic manifestations: unstable blood pressure, both racing and slow pulse rates, difficulty breathing, heat and cold intolerance, anxiety, plus a host of other symptoms. (See Chapter 17.)
- Immune imbalances may result in the development of food sensitivities, particularly to gluten. Some people also develop multiple chemical sensitivity syndrome (MCS). People with MCS react to low-dose exposures of chemicals such as perfumes, cleaning agents, and exhaust fumes, many of which are unavoidable in our current environment. (See Chapters 16 and 18.)
- Immune dysregulation often results in autoimmunity, in which the immune system attacks its own cells.
- Suppression of immune function from multiple tick-borne infections can lead to activation of microbes that were previously dormant. Many patients with Lyme disease complex experience reactivation of viral infections such as Epstein-Barr virus (EBV) and human herpes virus 6 (HHV6). (See Chapter 21.)
- People with chronic tick-borne infections seem particularly susceptible to complications from mold. Mold exposure is normally associated with respiratory symptoms such as congestion, sinus problems, and asthma; but reactions can also be systemic, resulting in migraine headaches, fatigue, joint pains, cognitive dysfunction, and depression. In other words, mold exposure can cause the same symptoms as Lyme disease complex. Complicating issues further, those molds most commonly associated with indoor water damage also excrete poisonous mold toxins. The symptoms of mold toxin exposure overlap with those of chronic infection, often resulting in severe inflammation and hormonal dysfunction, particularly suppressing the pituitary gland. (See Chapter 19.)
- Histamine reactions, either due to increased release of histamine into the circulation, decreased metabolism of circulating histamine, or heightened sensitivity to histamine, can add to inflammatory symptoms. This condition is referred to as mast cell activation syndrome (MCAS). (See Chapter 18.)
- Bb has an affinity for the nervous system, resulting in an array of neurological issues. A common problem is cognitive dysfunction, or brain fog, which, among other things, compromises the patient’s capacity to make good therapeutic choices and follow through on treatment regimens. This issue is exacerbated by sleep disorders. (See Chapter 17.)
- Bb and its co-infections, particularly Babesia and Bartonella, often cause neuropsychiatric disorders, particularly anxiety, depression, and irritability. Symptoms can be severe, resulting in panic attacks, suicidal ideation (and successful suicides), and rage episodes. It is important to realize that these problems are not only a secondary response to illness, they can be a direct result of infection causing neuroinflammation and neurotransmitter imbalance. (See Chapter 17.)
- People have very different physiologies, and their constitutions differ considerably. Genetic differences can impact detoxification, allergic dispositions, and autoimmune reactivity. There are also differences in each person’s immune system, impacting their individual capacity to contain and eliminate infections.
- By definition, people with Lyme disease complex have been sick for a long time. Many have been ill for years or decades before they receive a diagnosis, let alone find a practitioner willing to treat them. They often become weak and fragile, losing the rebound capacity of otherwise healthy people. As stated at the outset of this chapter, treating those with Lyme disease complex is complicated.
Risk factors of chronic disease
Prior or ongoing exposures to mold and mold toxins, heavy metals, and chemical volatile organic compounds (VOCs) vastly impact a person’s capacity to fight infection.
People also have enormously different tolerances to different antimicrobial agents, both herbal and pharmaceutical. Some patients have great difficulty taking any antimicrobials at all because they cannot tolerate the “die off,” also known as a Herxheimer reaction.
A history of emotional trauma can result in immune dysfunction and difficulty fighting infection. Social and emotional support structures have been shown to enhance emotional well-being and boost immune competence. Lack of support adds an extra hurdle to treatment. (See Chapters 1 and 2.)
Physicians are taught in medical school, “When a patient presents with multiple symptoms, search for the common denominator that explains everything.” This axiom applies well to acute illness: if a person has been healthy until two weeks ago and then develops fever, muscle aches, abdominal pain, nausea, and diarrhea, all these symptoms can be explained by a single pathogen.
Although Western medicine has done a good job of addressing acute illness, it has not been nearly as successful in addressing chronic disease. The “single-common-denominator” paradigm of illness no longer applies; there are usually multiple confounding issues. It takes detective work to uncover the assorted imbalances and restore people to good health.
Awareness of these tick-borne infections is critical; equally essential is recognition that every patient is unique. The seed is important, but understanding the soil is equally relevant. Lyme disease complex is complicated. It takes a persistent sleuth to help people get better.
Take home points
- Everybody is different, and treatment needs to be individualized.
- The diagnosis of acute Lyme disease is often missed for multiple reasons.
- Co-infections and toxic exposures increase the severity and duration of illness.
- Bb and co-infections may suppress immune function.
- Most people with Lyme disease complex have co-infections.
- Downstream issues of chronic infection complicate the clinical picture; endocrine, immunological, neurological, and gastrointestinal issues are common.
- Emotional stress can make recovery more difficult while social support can promote healing.
Editor’s note: Any medical information included is based on a personal experience. For questions or concerns regarding health, please consult a doctor or medical professional.