Gender bias is now a widely recognized problem in research. Sometimes this happens because women haven’t been studied in the first place. Even when they have been included in the research, their results may not be analyzed separately from those of men. Because of this, we don’t know much about how women differ from men in how they contract a disease, are diagnosed, or respond to treatment.
Is this an issue in Lyme disease? Are women more likely to get Lyme disease, more difficult to diagnose, or more prone to treatment failure? We decided to launch a research study using data from the MyLymeData patient registry. To kick off the study, we asked Dr. Raphael Stricker to explain how males and females with Lyme disease might differ. His video presentation is included below.
Lyme Disease Gender Differences
Dr. Stricker identified four major areas in Lyme disease where males and females are not alike:
- Women may attract more ticks and have more atypical Lyme rashes than men (Josek 2019).
- Commercial two-tier Lyme testing favors men over women, because men have more positive ELISA tests and more positive Western blots (Feder 1992, Rebman 2015, Schwarzwalder 2010).
- Women have an exaggerated response to Borrelia infection, with more inflammatory and inhibitory cytokines than men. This may promote the evolution of chronic Lyme disease. (Jarefors 2006).
- Women may have a higher treatment failure rate.
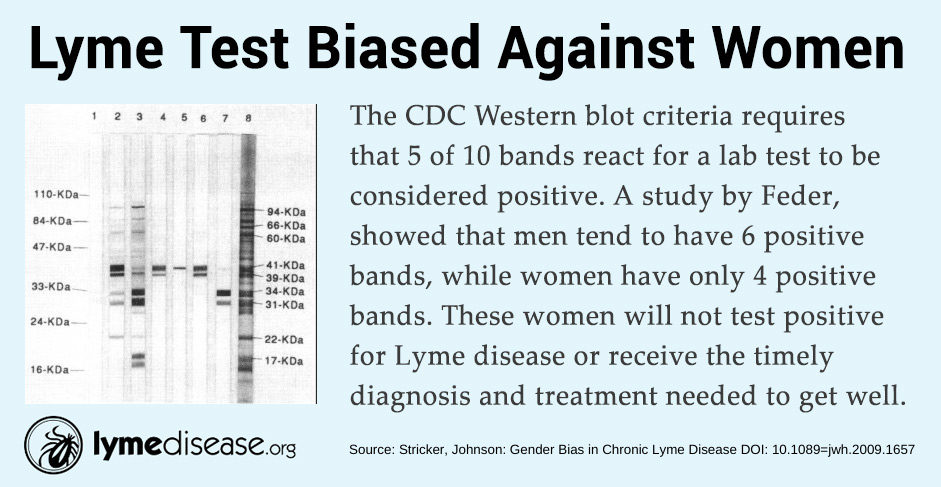
Lyme Tests Are Biased To Detect More Males
The CDC Western blot criteria requires that 5 of 10 bands react for a lab test to be considered positive. A study by Feder, showed that men tend to have 6 positive bands, while women have only 4 positive bands. These women will not test positive for Lyme disease or receive the timely diagnosis and treatment needed to get well (Stricker, Johnson 2009).
Lyme Disease Prevalence — Almost Twice As Many Females As Males
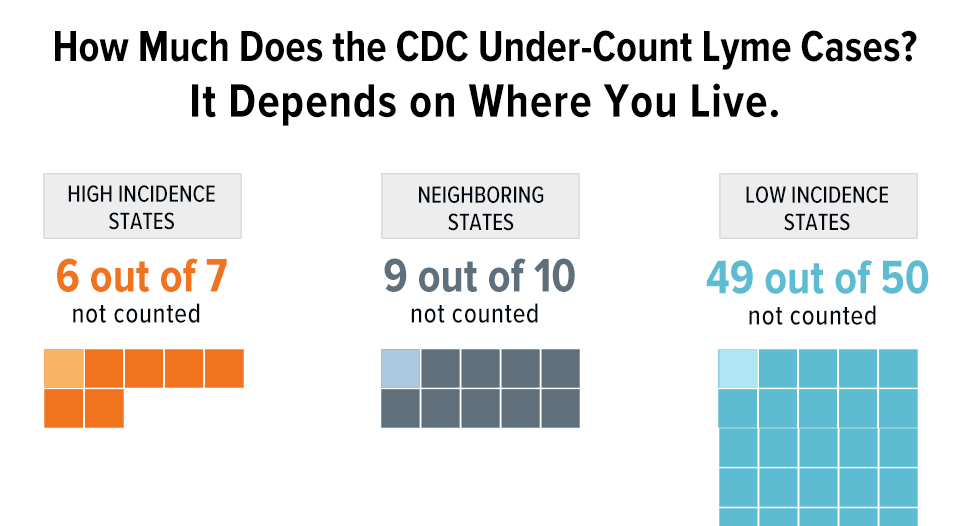
According to the CDC, most reported surveillance cases are male—58% males vs 42% females. The CDC statistics also show a bimodal distribution of Lyme disease — with children and adults over 50 reporting the most cases. Both of these assumptions have recently been called into question by other big data studies.
For example, FAIR Health, one of the largest insurance claims data bases, recently released a report on Lyme disease that shows more insurance claim lines with Lyme disease diagnoses were submitted for females than males and females do not have a bimodal age distribution. In fact, between the ages of 23-50, there were almost twice as many females as males with Lyme disease. (FAIR Health 2019).
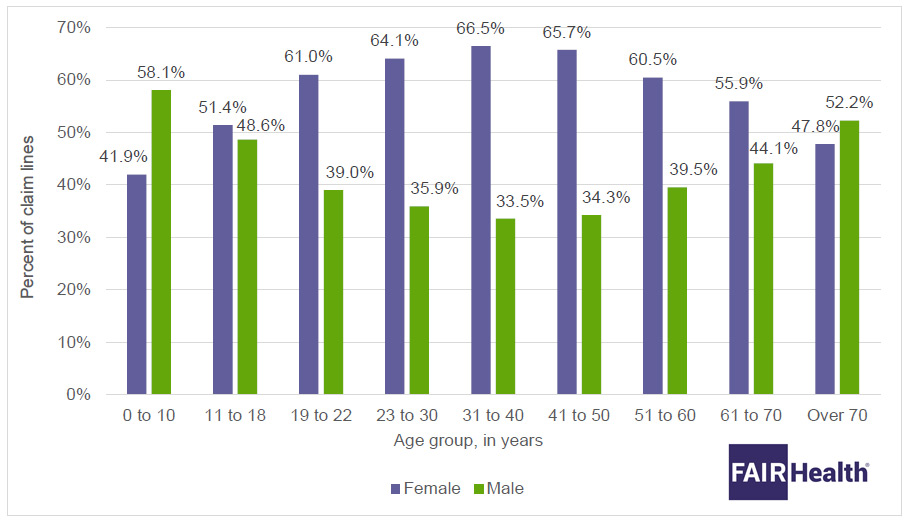
According to CDC data for 2017, among patients with reported confirmed and probable cases of Lyme disease, males predominated over females by 58 percent to 42 percent—nearly the opposite of FAIR Health findings.
— FAIR Health 2019.
FAIR Health researchers conclude that the difference between their statistical observations and those of the CDC stats may be due to the fact that FAIR Health data is from clinical practice, while CDC-reported cases are inherently skewed toward diagnosis based on lab tests. This result is similar to the findings reported in a Harvard study using Quest Lab data for Lyme disease. That study found that while males were more likely to have positive lab test results, overall, more females contracted the disease (Lee-Lewandrowski 2019).
Both the FAIR Health and Quest lab study support Dr. Stricker’s observation that Lyme lab tests favor males over females in terms of positive results. They also suggest that there may be considerable variation between the sexes in Lyme disease.
Research studies often exclude women because of pregnancy-related concerns. Or, they may simply neglect to take the extra step of evaluating differences between the sexes. Often what we “know” in science is based on men who participated in a study or averages across the sexes. As a result, we know very little about women. The end results is that “data can be sexist” as the Gates Foundation points out in its 2019 Annual Letter (Gates Foundation 2019).
Looking at the broader issue of gender bias in women, we are just now beginning to understand sex-based differences that may be key in medicine (Epstein 2019). For example, women having heart attacks are diagnosed less timely. Women are also 50-75% more likely than men to have adverse side effects from drugs (Epstein 2019). A recent article in Nature found that male and female mice have remarkably divergent biological pathways for pain – driven in part by distinct immune cell types and hormones (Dance 2019). Males and females also may respond to pain medications differently. As a result, drug companies are thinking about sex-specific pain treatments. Should we be looking at sex-specific antibiotics in Lyme disease?
Eighty-three percent of patients with persistent Lyme disease that are enrolled in MyLymeData are female. Our team of researchers is exploring MyLymeData to see what the data so graciously donated by patients might yield on the topic of gender bias in Lyme disease. We will be sure to keep you posted.
- Adrion et al, PLoS ONE 10:e0116767, 2015.
- Epstein, H. Medicine's Biggest Blind Spot: Women's Bodies. February 12, 2019, Society to Improve Diagnosis in Medicine https://www.improvediagnosis.org/dxiq-column/medicines-biggest-blind-spot-womens-bodies/
- FAIR Health, Trends and Patterns in Lyme Disease. An Analysis of Private Claims Data. White Paper. December 2019. https://www.lymedisease.org/wp-content/uploads/2019/12/FAIR_Health_White_Paper.pdf
- Feder et al, Clin Infect Dis 1992;15:788-93.
- Dance, A. Why the sexes don’t feel pain the same way. March 27, 2019. Nature. https://www.nature.com/articles/d41586-019-00895-3
- Jarefors et al, Immunology 118:224–232, 2006.
- Josek et al. Exp Appl Acarol. 77:59-64, 2019.
- Lee-Lewandrowski, et al, Am J Clin Pathol. 2019 Jun 5;152(1):91-96. doi: 10.1093/ajcp/aqz030.
- Rebman et al, Clin Rheumatol 2015;34:585
- Schwarzwalder et al, Gend Med 2010;7:320-9
- Stricker, Johnson: Gender Bias in Chronic Lyme Disease D01: 10.1089=jwh.2009.l657
If you are a patient who is not enrolled in MyLymeData, please enroll today. If you are a researcher who wants to collaborate with us, please contact me directly.
The MyLymeData Viz Blog is written by Lorraine Johnson, JD, MBA, who is the Chief Executive Officer of LymeDisease.org. You can contact her at lbjohnson@lymedisease.org. On Twitter, follow her @lymepolicywonk.